Reflections on February residency
We just wrapped up a whirlwind month in Richmond! We’re grateful to the many incredibly passionate people who have welcomed us to Richmond and shared their expertise in public health, civic technology, and community engagement. Our 27 days included:
 With our city partners, Danny Avula (Richmond City Health District) and Andreas Addison (Civic Innovator, City of Richmond)
With our city partners, Danny Avula (Richmond City Health District) and Andreas Addison (Civic Innovator, City of Richmond)| 95 | pages of Google doc notes |
| 48 | meetings |
| 6 | projects at the CodeAcross event organized by Code for RVA |
| 4 | days shadowing social workers and community health advocates |
| 1 | epic monster truck rally with the folks from the Richmond City Health District |
Here are a few takeaways from the month that will shape our thinking as we return to San Francisco to start building things.
There’s still a huge insurance gap in Virginia
Because Virginia did not expand Medicaid coverage under the Affordable Care Act, about 195,000 people fall in the gap between the maximum income for Medicaid eligibility and the minimum income needed to qualify for a subsidized private insurance plan. Uninsured and underinsured people in Richmond navigate a network of charity care options with varying costs and eligibility criteria.
It’s hard to keep track of all the available services, hard to figure out what you’re eligible for, and hard to apply
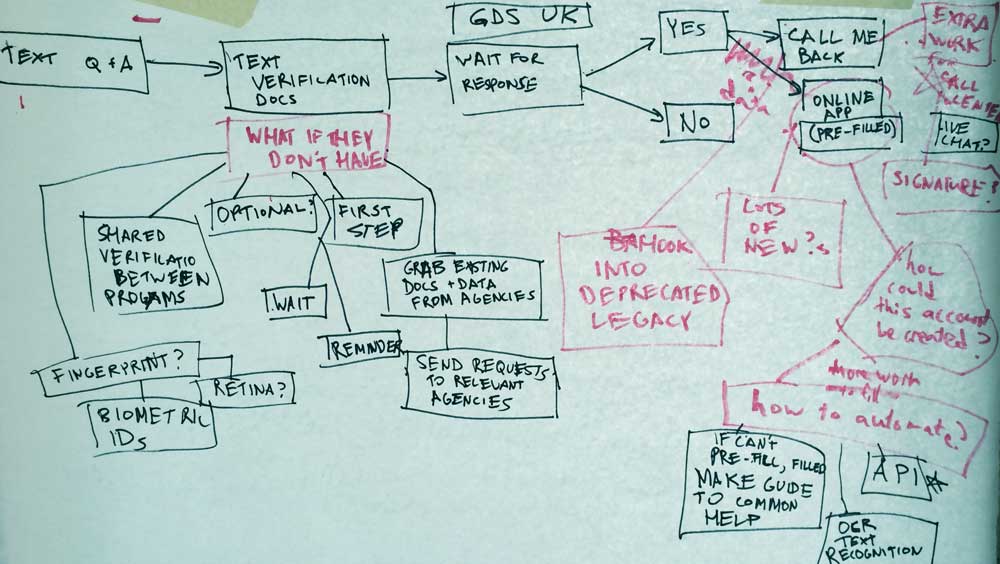 CodeAcross attendees mapped out SNAP eligibility screening workflows.
CodeAcross attendees mapped out SNAP eligibility screening workflows.The single most requested tool in our meetings was an up-to-date list of all available services for low-income people in Richmond. Because services change so quickly, existing resources like the statewide 211 system tend to have incomplete or out of date information. Eligibility criteria are often complex, and keeping track of all the documents needed to prove identity and income can be difficult. Patients often need to make an appointment for financial screening before they can receive care, or wait months to hear back after submitting an application.
Appointment scheduling is complicated
Making appointments often requires calling multiple offices to compare wait times, and keeping appointments can be difficult for people who have inconsistent work hours, unreliable transportation, and generally stressful lives. Patients want walk-in options, and many clinics provide them, but when demand exceeds capacity, people start lining up before sunrise and some are turned away.
Mental health is fundamental, but care is often difficult to access
Mental health problems can prevent people from accessing other health services or following doctors’ instructions, and they’re the number one reason for ambulance calls in Richmond. But only a few care options exist for people without insurance, and accessing them can require waiting months for an appointment.
For some, the ER is a better option than primary care
At a typical primary care clinic, there’s a two month wait for an appointment, each visit will cost $20, and you’ll need to go in for a financial screening before you can see a doctor. At the ER, you can walk in whenever you want and the visit will be free (the hospital will send bills later, but if you’re not concerned about your credit, you might ignore them). Plus, your family has been going to the ER for routine care your whole life, so the providers there are familiar. Where would you rather go?
Service providers struggle to communicate with each other efficiently
If a patient arrives at the emergency department of a hospital, the doctors there have information about the patient’s medical history at that hospital, but if the patient can’t tell them, they don’t know if the patient was seen recently at the city’s other health systems. They might order a test the patient already had done, or prescribe medications the patient is already taking. A clinic may refer a patient to a specialist, but not know whether the patient was ever seen. Nearly every clinician we met told us that electronic health record (EHR) systems “don’t talk to each other” and that this makes it more difficult for them to care for patients.
 Emma and Ben discussing project ideas with the Greater Richmond Patient Centered Medical Home Collaborative
Emma and Ben discussing project ideas with the Greater Richmond Patient Centered Medical Home Collaborative 